- March 17, 2022
- No Comment
- 13 minutes read
Seattle-area pet owners face long waits, and vet staff are burned out – The Seattle Times
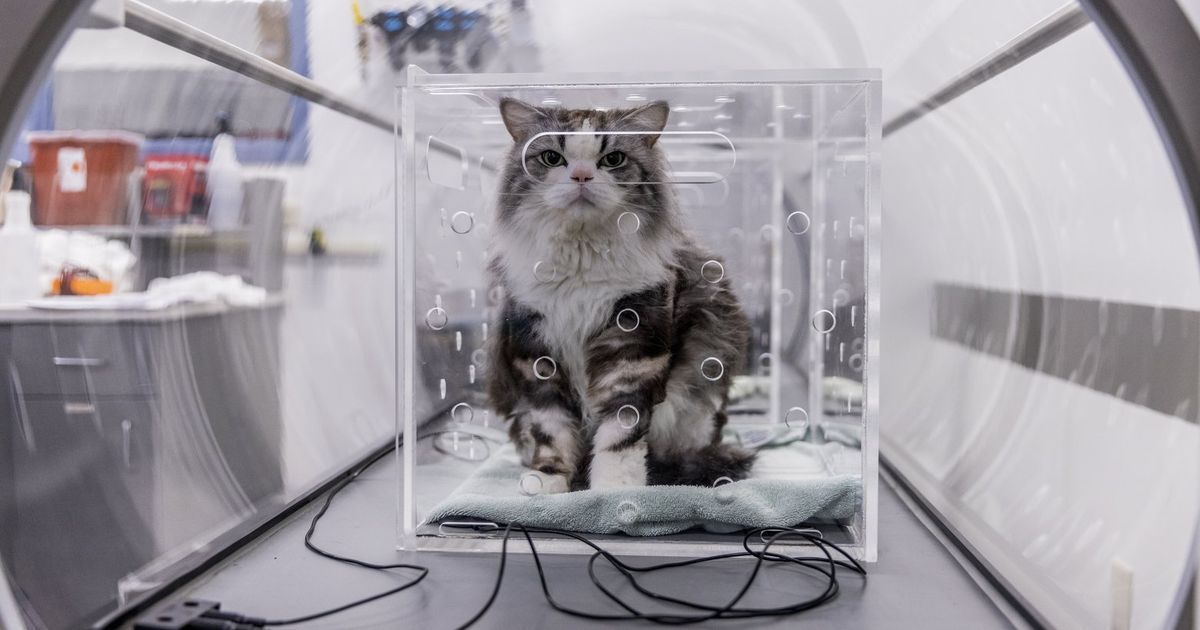
At the Animal Medical Center of Seattle, dogs (French bulldogs, Malteses, myriad doodles), cats (Siamese, shorthair) and humans (standard) are waiting for an employee to evaluate how long before each animal can get care.
Which of the 20 animals are most at risk? Today, staffers at the clinic can only see Priority 1 pets, those that could die without immediate intervention, and some animals likely to survive if care is given within hours.
Ailments include diabetes, acute kidney failure and seizures, and one canine ate sugar-free gum with xylitol, a toxic ingredient. A dog with a crushed chest is the most critical. Some will have to wait, potentially up to eight hours depending on their case.
“This is kind of tame, this is manageable,” says April Panpipat, the Shoreline animal hospital’s manager.
It may be considered tame now, but the number of calls and patients are an extreme change from before the COVID-19 pandemic, which caused new problems or exacerbated underlying issues facing the veterinary industry. Some days, several animals require one-on-one critical care and monitoring. Three or four patients may be dying at the same time.
The situation is much the same at animal hospitals and vet clinics throughout the region and nationally — long waits for appointments, high staff turnover and burnout, tense environments that required some providers to toughen their policies about owner behavior.
“I’ve worked in this profession for 20 years,” Panpipat said. “I never thought I would see the day where we would have to have diversion protocols and triage systems based on emergency situations … It’s a perfect storm put together.”
Bailey Verhunce woke up on a weekend morning and found Bodhi, her 3-year-old Doberman-greyhound mix named after Bodhizafa beer, covered in vomit and feces. He continued to decline as the hours wore on, “bleeding out both ends.”
Verhunce called 14 vets throughout the day, to no avail. The receptionist would ask if it was an emergency or if she could be put on hold, and initially, Verhunce said being on hold was fine, since Bodhi was still breathing. But then the calls would get disconnected or no one would come back — she waited 45 minutes for one to respond before giving up.
She downloaded Fuzzy, an app she had seen on Instagram that connects users with vet technicians and other vet services. The tech confirmed her fears.
“She basically said, ‘When you call you need to say this is an emergency, if it takes driving somewhere far, you need to get him seen, he needs to be seen immediately,’” Verhunce said.
Verhunce called five more providers and told them it was an emergency. They all said they were at capacity. One receptionist told her she didn’t know of any spots in King County that would take her dog. She made inquiries throughout the region, as far north as Mount Vernon. Nothing.
At 7 p.m., she got a lead: She called a Seattle emergency vet again, and the receptionist said to call back a bit later. She called back 90 minutes later, and was told to bring him in. But the wait would be six hours, they cautioned.
“We said whatever, this is the best we can do,” she said. “Meanwhile, Bodhi is declining and I am a hysterical dog mom.”
She packed the car with Bodhi, books and blankets and headed to the vet, then they waited. It was clear the employees were doing the best they could, Verhunce said. They eventually brought Bodhi in and ran tests, and diagnosed him with hemorrhagic gastroenteritis, a potentially life-threatening condition if left untreated.
At 2 a.m., with antibiotics and a nearly $1,000 bill, they headed home. It had been almost a full day since Verhunce first realized Bodhi was sick.
“There was a dog who came in shortly after Bodhi, with sutures that had come undone, and their wait was going to be at least eight hours,” Verhunce recalled. “It’s not as serious as some other emergencies, but eight hours? That broke my heart.”
The struggles facing animal care aren’t as simple as the oft-cited one of more pets, fewer staff. Experts say several factors are at play, with some a long time coming and others caused or exacerbated by the pandemic.
Data varies on whether there was truly a “pandemic puppy” boom. In the early months of the pandemic, the number of cat owners in Seattle increased by 18%, and dog owners increased by 4%, according to Nielsen, a market-research company. Nationally, the adoption rate of pets from shelters went up in 2020, but the number of adopted pets actually went down, because fewer shelter pets were available, according to the American Veterinary Medical Association (AVMA).
More time at home leads to more risks — a dog that would normally go to doggy day care instead could more easily get into a trash can at home and eat toxic raisins, for example. More people worked from home and spotted problems — real or imagined — during the day. One owner said his dog seemed lethargic in afternoons, but it turned out the dog just liked 3 p.m. naps.
Lockdowns bonded owners with their pets, which made a huge difference, said Dr. Alicia McLaughlin, the co-medical director of the Center for Bird and Exotic Animal Medicine in Bothell.
“I had multiple clients who said this little exotic pet is what kept me going for the past year,” she said. “They say, ‘I wouldn’t have survived the shelter-in-place without this little hamster.’”
Protocols to prevent the spread of COVID-19, like asking owners to stay outside, sanitizing rooms and having fewer people in a building, affected clinics’ efficiency. In 2020, productivity, measured by the average number of patients seen per hour, decreased by 25%, according to the AVMA.
That doesn’t mean anyone was working less, said Candace Joy, CEO of the Washington State Veterinary Medical Association, in an email. Joy compared the situation to walking a mile on a treadmill versus a mile on a beach.
Even a slight uptick in animals needing to be seen, combined with a decrease in the number of patients per hour, can create a significant backlog, the AVMA wrote in a September report.
Meanwhile, providers lost staff for pandemic-related reasons. Some employees had to quit because they couldn’t find care for their children at home, others got COVID-19 themselves or needed to assist a loved one who contracted the coronavirus.
There are about 2,050 veterinarians in Washington and 2,230 vet techs, according to the U.S. Bureau of Labor Statistics, and staff turnover has historically been high in the physically and emotionally taxing profession. The average turnover for a vet tech, for example, is five years, according to Dr. Dori Borjesson, dean of Washington State University’s College of Veterinary Medicine. Pay has been one factor — the median wage in Washington for a vet tech is $41,150, according to labor bureau statistics.
Prospective veterinarians face financial and capacity barriers: There are only about 30 vet schools nationally, and WSU’s acceptance rate is less than 10%. The average debt load is $126,000 after four years of education. But Borjesson said she tells students there is no better time to be a vet, because there are more locations and options for them than ever before.
Among the 70-plus hospitals in the VCA Animal Hospitals network’s northwest region, there are 100 openings for veterinarians alone, according to Dr. Stanley Rubin, regional medical director for Washington, Oregon, Alaska and Idaho.
“COVID made a problem that we were anticipating surface and show its ugly head,” he said.
The pandemic also necessitated canceling or delaying routine appointments. Jason Svatos of Seattle tried to make a teeth-cleaning appointment for his cat Trillian in July, but was given only one option: Oct. 7. He couldn’t make that date, so now he’s looking in February 2022.
“Scheduling something that far in advance is tough anytime, let alone when there’s an active pandemic and you have no idea what the next two weeks will look like, let alone three or four months,” he said.
Issues that would have required a short stay one month might be overlooked and turn into an emergency later. Or an owner might not be able to find a timely appointment at their regular vet, so they go to an ER. That adds to ER wait times and volumes, and costs more.
“If a dog has an ear infection, you can’t wait two months, so you have to go to an ER,” said Rae Thompson, a vet tech in a Puget Sound emergency clinic. “And you can go, but we are also trying to see a dog hit by a car. And sometimes we have 10 or 12 people arrive in 60 minutes. If you spend one hour on a pet, per pet, that’s a whole day’s worth that has already arrived by 10 a.m. And the calls keep coming.”
To show owners how busy all providers were, Thompson created a spreadsheet with emergency vet wait times, which she posts daily to Instagram and Facebook. On a Monday afternoon, the times ranged from zero to three hours at a clinic in Pasco to 12-plus hours in Mount Vernon. Out of two dozen facilities, five were at capacity and diverting patients to other sites.
Vet staff recommend owners not wait to find care for their pet, so there’s some leeway if there aren’t any appointments available for a few days.
Try to establish a relationship with a general practice vet, so the provider might be more likely to squeeze in an appointment in an emergency. They also recommend calling pet poison control hotlines or looking up apps that offer telehealth, though that can be harder for animals than humans.
But don’t hesitate to go to the ER if you’re worried, they said.
“You may have to wait longer in line in the ER if your pet is less sick,” veterinary technician Rae Thompson said. “But it will probably be a better outcome than if you wait and your pet is critically ill and there is nothing available.”
More
It’s not unusual for vet staff to have to call the police at the Animal Medical Center. Owners have screamed at workers, thrown clipboards and ripped everything off the counters. They hired a security guard. At the Center for Bird and Exotic Animal Medicine, a client told a staff member they should consider a different field because this was something they didn’t excel at. The facility added a sign on the front door that physical and verbal abuse wouldn’t be tolerated.
Tempers flare outside vet buildings as stressed owners are told bad news about their pet. Curbside service makes this more difficult — it’s easier to lash out when you can’t see someone’s face. Owners might not understand the long waits since they can’t see what is happening inside. They’re scared and may see any obstacle, such as costs or wait times, as a direct opposition, said Dr. Meera Music, co-medical director of the Center for Bird and Exotic Animal Medicine.
Music once had a client scream at her because she had to wait several hours. Music replied that the reason for the wait was that Music had been walking through euthanasia options for six other grieving patients.
They might not see the full picture of what the vet staff are dealing with, but owners’ experiences and emotions are on display as they wait. While waiting outside BluePearl in Renton with her French bulldog Rosemary, Jenna Abts watched as an owner sprinted from their car to the doors with an unresponsive black and white cat. A family got out of an SUV and surrounded a dog lying in a bed, waiting for what was going to be a last visit.
“It wasn’t unusual that these things happen at Blue Pearl, but what was unusual was how visible the tragedies were — there just wasn’t anywhere else for people or their pets to be,” Abts wrote in an email.
When Abts stepped inside to use the restroom, a vet tech at the desk remembered Abts and the family’s other French bulldog, Basil.
“I am constantly in awe at how the staff there hold it together, and could even possibly recall a pet and owner given the sheer volume of visits they have every day,” Abts said. “I cannot imagine the emotional and physical stress they’re under.”
The opinions expressed in reader comments are those of the author only and do not reflect the opinions of The Seattle Times.

